
For Providers: Effective Female Fertility Testing with the Parryscope Technique
Quick look at Parryscope female fertility testing
Parryscope® female fertility testing technique is a fast, accurate in-office method of testing fallopian tube patency that is similar to a hysterosalpingogram (HSG) test, but with significant improvements.
The Parryscope technique is best described as flexible hysteroscopy combined with sonosalpingography, where the air bubbles in saline visualized passing through the fallopian tubes on sonosalpingography are seen entering the ostia hysteroscopically.
The primary benefit of the Parryscope technique is assessment of fallopian tube patency. However, when combined with sonography for antral follicle count for ovarian reserve, sliding sign for adhesions and uterine anatomy beyond hysteroscopy, the broader understanding obtained is what we refer to as the Parryscope approach. Though we prefer combining sonography and hysteroscopy to rapidly get a reasonable sense of a patient’s fertility, even using just a hysteroscope for the Parryscope technique allows:
- Gentler patient care than with HSG
- High accuracy
- Fast results (<5 minutes for the Parryscope technique on average)
- Single visit testing
- Fertility evaluation patients highly prefer over HSG.z
For an appointment, contact us online or call 888-4PR-SCPE (477-7273)
Related resource: What Is Parryscope Fertility Testing?
Why consider Parryscope female fertility testing instead of HSG for your patients?
Clinicians want the best possible care for their patients. A single test that accurately, gently, quickly and safely assesses female fertility in a single visit would be a great step forward for the field of infertility. This is what can be achieved through the Parryscope approach, invented by Dr. John Preston “Pres” Parry.
Clinical advantages of Parryscope over HSG
The Parryscope technique provides clinical advantages over HSG. First, it can be done conveniently in a typical provider examination room, without X-ray equipment or radiology support staff.
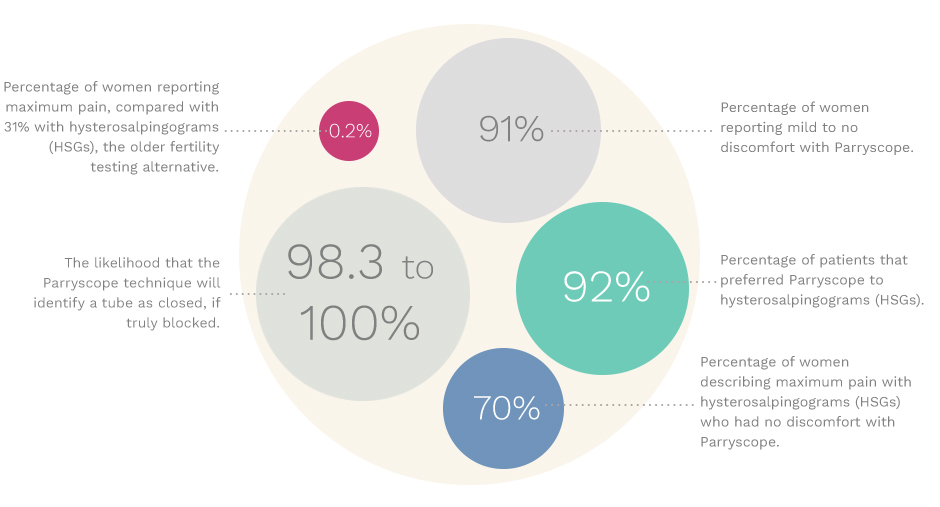
The Parryscope’s efficacy was demonstrated in a study to determine whether air bubbles infused into saline during flexible office hysteroscopy can accurately predict tubal patency. This study conducted by Dr. Parry and others involved 435 patients who underwent office hysteroscopy with air infusion, 89 of whom also had abdominal surgery. The results showed:
- Sensitivity to tubal occlusion was 98.3 to 100 percent
- Specificity was 83.7 percent with standard chromopertubation pressures
- 95.3 to 100 percent of the time proximal patency was observed, whole tubal patency was observed through chromopertubation for patients with surgical data.
The study’s conclusions: “Air-infused saline at office hysteroscopy can accurately assess tubal patency. Additionally, bilateral patency identified through office hysteroscopy may predict bilateral patency at surgery better than several commonly used historic and sonographic variables.”
Preliminary findings were presented at the 2015 annual meeting of the American Society for Reproductive Medicine (ASRM) with subsequent publication of the full sample in the Journal of Minimally Invasive Gynecology article, “Proximal Tubal Patency Demonstrated Through Air Infusion During Flexible Office Hysteroscopy Is Predictive of Whole Tubal Patency.”
For Dr. Parry’s Detailed Study:
- See the Full Article in the Journal of Minimally Invasive Gynecology
- See the Full Article in Fertility & Sterility
- Watch Dr. Parry’s video: Performing the Parryscope technique gently for office tubal patency assessment
Proven less painful: Parryscope technique is gentler for and preferred by patients
The Parryscope technique’s single clearest advantage is how gentle it is for patients, as demonstrated in another study published in Fertility and Sterility. Patients experience far less pain with hysteroscopic evaluation than with HSG, and this with only a third of them using OTC pain relief prior and almost none using stronger medications.
In the study the Parryscope technique resulted in 110-fold lower likelihood of maximum discomfort than with HSG.
Reducing pain and discomfort with the right tools and technique
A 2.5 mm flexible, pediatric hysteroscope is critical to reducing pain by not requiring dilation and because it reduces abrasion of the cervical side walls that could cause discomfort. The smaller the hysteroscope, the greater the amount of space around it relative to the cervix, permitting saline outflow, which is particularly important for patients with bilateral tubal occlusion (inflow without outflow leads to pain).
Large caliber hysteroscopy can create greater discomfort, particularly in patients with a nulliparous cervix and particularly if a patient has had previous cryotherapy or chlamydia cervicitis. Also, because the patient should empty her bladder prior to hysteroscopy to allow air bubbles to rise to the ostia, the sharp anteflexion of the uterus can lead to greater discomfort with a rigid hysteroscope.
The gentle Parryscope technique also seems to have a low rate of tubal spasm, and transient relaxation of spasm is readily observed. Core considerations for gentle technique to reduce spasm include small caliber, flexible hysteroscopes and avoiding over distention, an important source of pain in HSG and sonosalpingography approaches that occlude outflow of dye or saline.
Compare with HSG fertility testing
Comparison of pain relative to hysteroscopy was done at the time of hysteroscopy for almost all patients who had HSG. The following charts indicate the improved gentleness with Parryscope technique and its acceptance by patients.
Pain |
Parryscope (435) |
HSG (74/435) |
|---|---|---|
| None | 54 % | 12 % |
| Minimum | 24 % | 7 % |
| Mild | 12 % | 7 % |
| Moderate | 8 % | 18 % |
| Severe | 0.9 % | 12 % |
| Maximum | 0.2 % | 31 % |
For patients with maximum discomfort with HSG
- 70 percent had no pain with Parryscope
- 96 percent had mild to no pain with Parryscope
For patients having both HSG and Parryscope
- 85 percent strongly preferred Parryscope
- 7 percent somewhat preferred Parryscope
- 4 percent had no preference
- 4 percent slightly or somewhat preferred HSG
Contact Dr. Parry to discuss referring your patients for Parryscope female fertility testing
How the Parryscope female fertility testing technique is performed
Before screening, the patient should have a negative pregnancy test and be examined for other issues that might preclude testing, as well as provide consent. If the patient is high risk for sexually transmitted infections (STIs), doxycycline may be considered.
Parryscope testing includes the following steps
- Setup: Basic components include a sterile 0.9 percent sodium chloride solution, IV tubing with a drip chamber, a speculum and a flexible office hysteroscopy setup.
- Speculum placement. (Vaginoscopy without a speculum can also be performed.)
- Chlorhexidine preparation of the cervix.
- Start saline flow. Many women do well when there is a stream that forms a 90-degree angle 2 cm away from the tip of the hysteroscope (not so slow as to drip, not so fast as to be “shooting out” in a straight line). However, this should be adjusted based on distention and patient comfort as well as anticipated cervical caliber.
- Advance the flexible hysteroscope into the uterus.
- Fully visualize the uterine cavity. Dr. Parry prefers assessing the uterine cavity for at least 10 seconds before adding bubbles to allow pressure equilibration.
- Briefly invert the nearly empty drip chamber so that ¼ mL of air (which is approximately 3 cm in typical IV tubing) is added to the line. With a slower rate of flow, one may need to invert the column longer. 5-10 mL or more can be used for sonosalpingography and 2-5 mL is introduced intravascularly for echocardiogram.
- Brief flicking of the column causes a finer stream of bubbles, allowing for better bilateral dispersion. Without being able to see past the ostia, some might be concerned that air bubbles could accumulate in hydrosalpinges falsely suggesting patency, but this hasn’t been an issue in our studies.
- Beyond needing an empty bladder so air bubbles rise to the ostia, if the air bubbles are preferring one side, patients may have to roll their hips so air bubbles are adjacent to the ostia. Stabilizing the hysteroscope with the nondominant hand against the perineum helps avoid removal of the hystersocope during this repositioning.
- Observe air bubble dispersion for patency, with observation up to 40 seconds if not advancing through the ostia on a particular side.
- Remove the hysteroscope and speculum.
Next steps: Refer your patient to Dr. Parry for Female fertility testing
Dr. Parry is now offering the Parryscope technique and approach in multiple states. Contact him today to refer or discuss performing this test on your patients.
