
What is Parryscope Fertility Testing?
A breakthrough in female fertility testing, the Parryscope approach gives a comprehensive, gentle view of fertility in only 15 minutes.
Though testing whether the fallopian tubes are open has traditionally been done with hysterosalpingograms (HSGs), the Parryscope® approach provides significant improvements and benefits. These include minimal discomfort, high accuracy, thorough testing, a quick procedure with instant results, and improved safety.
For an appointment, contact us online or call 888-4PR-SCPE (477-7273)
What is the Parryscope fertility test?
The Parryscope is Dr. John Preston “Pres” Parry’s patent-pending fast, effective and gentle testing method that evaluates the core aspects of female fertility – ovarian reserve, fallopian tube patency (meaning whether the tubes are open so sperm and egg can meet) and uterine factors – in a single diagnostic procedure.
Just as important as the test itself, Parryscope fertility testing includes Dr. Parry’s discussion of results in the same appointment, using easy-to-understand language and providing clear guidance on next steps.
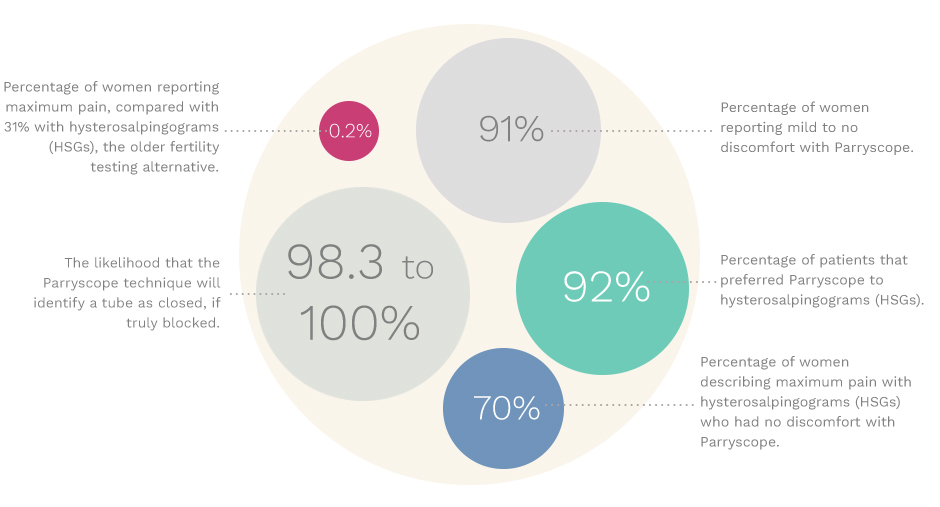
Perhaps the single greatest advantage of the Parryscope technique is how gentle it is relative to other methods, such as HSG testing. In our detailed study of the Parryscope technique compared with HSG, 99 percent of women described their discomfort as moderate to none and 91 percent as mild to none. Only 0.2 percent experienced maximum pain with the Parryscope technique, compared with 32 percent of women who experienced the maximum level of pain with HSG.
The goal of our test is to quickly identify a woman’s chances for pregnancy and to help her decide whether she should continue with natural conception, try oral medication and insemination, or move on to an assisted reproductive technology, such as in vitro fertilization (IVF).
Three female infertility tests in one
The Parryscope approach evaluates three critical factors in a woman’s fertility.
- Are there a reasonable number of eggs? To determine this, we use ultrasound to perform an antral follicle count for the ovaries. Antral follicles are small sacs filled with fluid that contain an immature egg. We measure and count the antral follicles in both ovaries to learn if the ovarian reserve (number of potential eggs remaining in the ovaries) is low, normal or robust.
- Can sperm and eggs meet in the fallopian tubes for fertilization? Using Dr. Parry’s special Parryscope technique, we determine whether one or both fallopian tubes are blocked or damaged. Blocked or damaged fallopian tubes can affect pregnancy chances in two ways: by preventing sperm from reaching the egg for fertilization and/or preventing a fertilized egg from reaching the uterus for implantation. Also, when combined with ultrasound, the approach can sometimes identify whether there is scarring in the pelvis that might reflect previous infection, endometriosis or other problems.
- Is the uterus favorable for embryo implantation and successful pregnancy? Using ultrasound with the special thin and flexible hysteroscope, we get a thorough view of the uterus and can evaluate its ability to accept and nurture the embryo. This is crucial, as many instances of infertility are due to a woman’s fertilized egg failing to implant in the uterus for development. Issues with the uterus may also cause miscarriages after pregnancy (also known as recurrent pregnancy loss), which can be a problem distinct from infertility.
How Dr. Parry evaluates the fallopian tubes through the Parryscope technique
The Parryscope screening is typically done on days 7-11 of the menstrual cycle, with day 1 being the first day of full, heavy flow (the start of a woman’s period). This timing means the uterus’ lining has shed, allowing one to see inside well. This also allows blood to clear, without allowing too much time for the lining to regrow.
Prior to testing the fallopian tubes, we confirm that the patient is not pregnant and look for factors that might suggest we shouldn’t perform the test. We also use ultrasound to evaluate the pelvis, including the ovaries, uterus, and seeing if the fallopian tubes are blocked and filled with fluid (hydrosalpinges). If these are found, it doesn’t automatically prevent further testing, but antibiotics may be discussed.
For the hysteroscopic (fiberoptic) portion, the Parryscope technique involves gently inserting the small hysteroscope vaginally past the cervix and into the uterus. It also involves use of a saline solution to expand the uterus. While looking in the uterus with the hysteroscope, we release air bubbles that travel to or through the ostia, which is where the fallopian tubes connect with the uterus.
If the bubbles enter the ostia, the fallopian tubes are almost always open. If the bubbles do not pass, while this doesn’t guarantee the tube is blocked, it makes us a lot more suspicious, particularly if a woman’s history or other ultrasound findings suggest risk for blocked tubes.
Benefits of Parryscope fertility testing
Though HSGs have been performed on women for over 100 years, it is arguable as to how much that test has advanced over that time. For women who have had both HSG and the Parryscope technique, 85 percent strongly preferred the Parryscope technique over HSG and 92 percent somewhat or strongly preferred it.
Though less pain is valuable in itself, the Parryscope technique seems to provide another advantage of reducing the risk for tubal spasm. Painful testing can cause the uterus to clamp down around the tubes, potentially making a tube or tubes appear closed when they are actually open.
Other benefits of this breakthrough test, include:
- It’s fast, providing most women with what they need to know about their own fertility in a 15-minute procedure
- It’s accurate
- It is very gentle
- Clear results help with future decision making
- It seems as safe if not safer than alternative approaches, with likely fewer infections and vasovagal events (passing out)
- Cervical dilation, which can be painful as well as make holes in the uterus, is less likely with this approach
- It avoids radiation/X-rays
- It uses air and saline, unlike HSG that can use dyes that result in allergic reactions.
TRUTH IN NUMBERS
Parryscope fertility testing study
Who should consider the Parryscope approach?
This test can be considered by any woman who needs fertility testing or is curious about her fertility and has other reasons for pelvic evaluation. If a woman has an active pelvic infection, this will need to be cleared up before testing. Also, women with a backward tipped (retroflexed) uterus and previous tubal ligation with reversal may not be as good candidates as others for this test.
Related Resources
Parryscope fertility testing risks
In rare cases, infection may occur. Some women may experience discomfort, but most do not. In our study, 99 percent of women described their discomfort as moderate to none, and only 1.1 percent experienced severe or maximum pain.
Patients should be aware that no test is 100 percent accurate, nor can any test guarantee that a woman will or won’t get pregnant. However, the Parryscope approach can instantly generate answers for many women about issues they’ve faced for years. So while there are risks to any procedure, there are also risks to not understanding one’s body through accurate testing.
Next steps: Schedule an initial Parryscope consultation
If you feel infertility is blocking your way to building your family, contact us today to schedule testing with Dr. Parry. After the quick and gentle evaluation, he will take the time to explain your results and give you a clear understanding of how to move forward on your journey to building your family.
